Have you ever wondered how the human heart, a remarkable organ, develops and functions? And what happens it’s defected?
Let’s explore the world of congenital heart defects (CHD), a condition that affects thousands of individuals worldwide. Heart Symptoms CHD is a type of birth defect that occurs when the heart or blood vessels near the heart do not form properly during Pregnancy Heart Attack pregnancy.
What exactly is a congenital heart defect, and how does it impact the lives of those affected?
Table of contents
What is Congenital Heart Defect?
At the core of our existence lies the heart, a vital organ responsible for pumping blood and sustaining life. A congenital heart defect refers to an abnormality in the structure or function of the heart that exists from birth. These anomalies can manifest in various forms, affecting the heart’s chambers, valves, or blood vessels.
How common are Congenital Heart Defects?
Contrary to popular belief, congenital heart defects are not as rare as one might think. Approximately 1 in every 100 babies is born with a congenital heart defect. Heart health Congenital heart defects can range in severity from mild to life-threatening, and the symptoms and treatment options can vary widely depending on the specific type of defect. The prevalence of CHD underscores the importance of understanding the condition and its potential impact on individuals’ lives.
Types of Congenital Heart Defects
Congenital heart defects (CHDs), come in several distinct types, each presenting unique challenges and requiring specialized medical attention.
Listed below are the types of congenital heart defects:
- Atrial Septal Defects (ASD): ASD involves a hole in the septum (the wall) between the heart’s upper chambers (atria). This opening allows oxygen-rich blood to mix with oxygen-poor blood, affecting the heart’s efficiency.
- Ventricular Septal Defects (VSD): VSD is characterized by a hole in the septum between the heart’s lower chambers (ventricles). This condition leads to the mixing of oxygenated and deoxygenated blood, placing strain on the heart and potentially causing complications.
- Tetralogy of Fallot: This complex congenital heart condition comprises four abnormalities: a ventricular septal defect, pulmonary stenosis (narrowing of the pulmonary valve and artery), an enlarged right ventricle, and an overriding aorta. Tetralogy of Fallot can result in decreased oxygen levels in the blood.
- Coarctation of the Aorta: In this defect, the aorta, the main artery carrying oxygenated blood from the heart, is narrowed or constricted. This constriction can impede blood flow to the lower part of the body, leading to various complications.
- Patent Ductus Arteriosus (PDA): PDA occurs when a blood vessel, the ductus arteriosus, fails to close after birth. This vessel, essential during fetal development, can cause abnormal blood flow and stress on the heart if it remains open.
- Transposition of the Great Arteries: In transposition of the great arteries, the aorta and pulmonary artery are switched, leading to improper circulation of oxygenated and deoxygenated blood. This condition requires corrective surgery early in life.
Symptoms of Congenital Heart Defect
While some CHDs may go unnoticed for years, others manifest through distinct symptoms that, if identified early, can lead to timely intervention and improved outcomes.
Here are the symptoms of congenital heart defect:
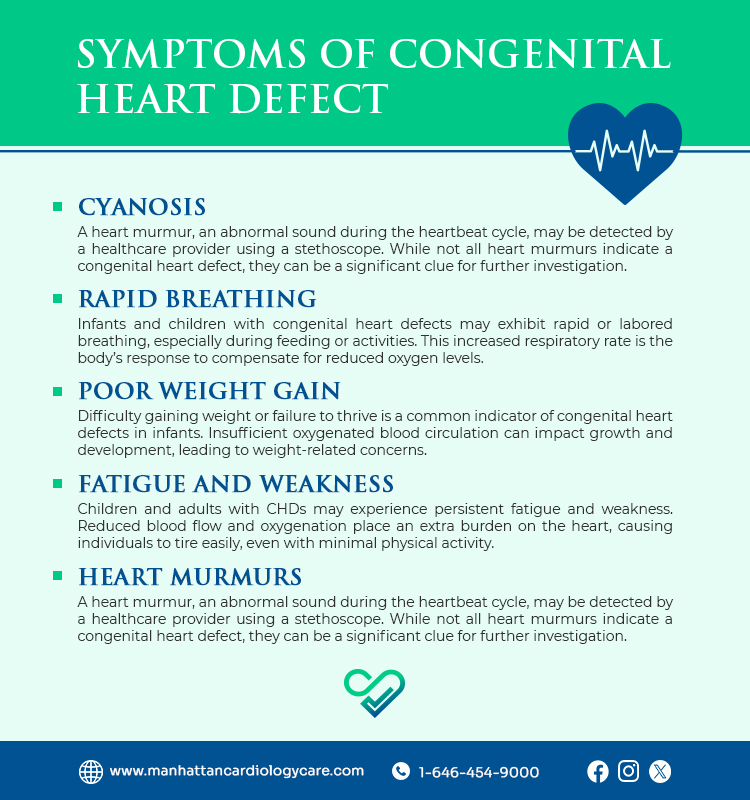
- Cyanosis: One of the hallmark symptoms of CHD is cyanosis, a bluish tint to the skin, lips, or nails. This discoloration results from inadequate oxygen levels in the bloodstream and may be more noticeable during physical exertion or periods of stress.
- Rapid Breathing: Infants and children with congenital heart defects may exhibit rapid or labored breathing, especially during feeding or activities. This increased respiratory rate is the body’s response to compensate for reduced oxygen levels.
- Poor Weight Gain: Difficulty gaining weight or failure to thrive is a common indicator of congenital heart defects in infants. Insufficient oxygenated blood circulation can impact growth and development, leading to weight-related concerns.
- Fatigue and Weakness: Children and adults with CHDs may experience persistent fatigue and weakness. Reduced blood flow and oxygenation place an extra burden on the heart, causing individuals to tire easily, even with minimal physical activity.
- Heart Murmurs: A heart murmur, an abnormal sound during the heartbeat cycle, may be detected by a healthcare provider using a stethoscope. While not all heart murmurs indicate a congenital heart defect, they can be a significant clue for further investigation.
Causes of Congenital Heart Defect
Listed below are all the possible causes of congenital heart defects.
- Genetic Factors: A significant number of congenital heart defects have a genetic component. Changes or mutations in specific genes responsible for heart development can lead to structural abnormalities. In some cases, these genetic variations may be inherited from one or both parents, increasing the risk of CHDs in subsequent generations.
- Environmental Influences: Prenatal exposure to certain environmental factors can impact fetal heart development. Factors such as maternal infections, exposure to certain medications, or the use of substances like alcohol and tobacco during pregnancy have been linked to an increased risk of congenital heart defects. Avoiding these potential teratogens can contribute to minimizing the risk.
- Maternal Health During Pregnancy: The health of the mother during pregnancy plays a crucial role in fetal development. Certain maternal conditions, such as diabetes, obesity, or poorly controlled phenylketonuria (PKU), can elevate the risk of congenital heart defects. Adequate prenatal care, including proper management of existing health conditions, is essential for reducing these risks.
- Chromosomal Abnormalities: Disorders involving chromosomal abnormalities, such as Down syndrome (Trisomy 21), are associated with an increased incidence of congenital heart defects. The intricate genetic interplay during fetal development means that anomalies in chromosome number or structure can contribute to heart abnormalities.
- Unknown Factors: In some cases, the precise cause of congenital heart defects remains unknown. Researchers continue to explore and unravel the complex interactions of genetic and environmental factors that contribute to these anomalies. Ongoing studies aim to shed light on these mysteries, paving the way for improved prevention and intervention strategies.
Treatments for Congenital Heart Defect
Understanding the treatment modalities is crucial for individuals with CHDs, their families, and healthcare providers. Let’s explore the diverse treatment options used to address congenital heart defects:
- Medications: In some cases, congenital heart defects may be managed through medications. These drugs aim to alleviate symptoms, regulate blood pressure, or enhance heart function. Medication plans are often personalized based on the individual’s specific condition and overall health.
- Catheter Procedures: Minimally invasive catheter procedures have revolutionized the treatment of certain congenital heart defects. Using a catheter threaded through blood vessels, interventional cardiologists can repair or close defects, such as atrial septal defects or patent ductus arteriosus, without the need for open-heart surgery.
- Surgery: For more complex congenital heart defects, surgical intervention may be necessary. Skilled cardiac surgeons can repair structural abnormalities, close septal defects, or reconstruct heart valves. Advances in surgical techniques and technology have significantly improved the outcomes of congenital heart surgeries.
- Heart Transplant: In severe cases where the heart’s structure is significantly compromised, a heart transplant may be considered. This involves replacing the damaged heart with a healthy donor heart. While this option is reserved for specific situations, it can offer a new lease on life for those with end-stage congenital heart defects.
Living with CHD
Coping with congenital heart defects is a lifelong journey that requires resilience and support. Patients and their families should be aware of the potential challenges and embrace a heart-healthy lifestyle to enhance overall well-being.
When to See a Doctor?
Timely medical intervention is crucial for individuals with congenital heart defects. Regular check-ups, monitoring of symptoms, and prompt medical attention can significantly improve the quality of life for those affected. Types of Heart Failure Early diagnosis and appropriate treatment are essential in managing congenital heart defects, as the condition can lead to various complications if left untreated.
Frequently Asked Questions
What is the most common congenital heart failure?
The most common congenital heart defect is Ventricular Septal Defect (VSD), which involves a hole in the septum between the heart's lower chambers.
What is the most complex congenital heart defect?
Tetralogy of Fallot is considered one of the most complex congenital heart defects. It involves four distinct abnormalities, impacting the heart's structure and function.
Can you live with a congenital heart defect?
Yes, many individuals with congenital heart defects can lead fulfilling lives with proper medical management and, in some cases, intervention through medications, procedures, or surgery. Regular monitoring and care are crucial for maintaining optimal heart health.
– Disclaimer –
This blog is for informational & educational purposes only, and does not intend to substitute any professional medical advice or consultation. For any health related concerns, please consult with your physician, or call 911.