Table of contents
What is a Heart Attack?
A heart attack, scientifically known as myocardial infarction, occurs when the blood flow to a section of the heart muscle is obstructed, usually by a blood clot. This interruption deprives the heart tissue of oxygen and can lead to its damage or death.
Common Warning Signs of a Heart Attack
Recognizing the common warning signs of a heart attack is immensely important for effective management. Heart condition The typical symptoms of a heart attack include chest pain or discomfort, shortness of breath, cold sweats, nausea, and lightheadedness. Prompt medical attention is crucial, as rapid treatment can minimize the damage to the heart muscle and improve the chances of survival. While heart attack symptoms can vary, here are the typical indicators to be vigilant about:
- Chest Discomfort: Uncomfortable pressure, fullness, squeezing, or pain in the center of the chest.
- Shortness of Breath: Difficulty breathing or a feeling of breathlessness, even at rest.
- Upper Body Discomfort: Pain or discomfort in the arms, back, neck, jaw, or upper stomach.
- Cold Sweats: Profuse sweating, often accompanied by clammy skin.
- Nausea or Vomiting: Feeling nauseous, possibly leading to vomiting.
- Lightheadedness or Dizziness: Feeling faint, lightheaded, or dizzy.
- Fatigue: Unusual and extreme tiredness, even with minimal exertion.
What Does a Heart Attack Feel Like?
Experiencing a heart attack may involve sensations like heavy chest pressure, radiating pain to the arms or jaw, shortness of breath, nausea, cold sweats, lightheadedness, and overwhelming fatigue. It’s essential to recognize these heart attack symptoms promptly and seek immediate medical attention. Heart Attack And Cardiac Arrest A heart attack is different from cardiac arrest, which is the sudden and complete loss of heart function, often resulting in immediate unconsciousness and the absence of a pulse.
Heart Attack Symptoms in Women vs Men
While both men and women may experience similar heart attack symptoms, there are notable differences in how these signs manifest. Recognizing these differences is crucial for accurate diagnosis and timely medical intervention.
Common Symptoms in Both Genders:
1) Chest Discomfort:
- Men: Often described as pressure, tightness, or pain.
- Women: Can be subtler, with discomfort or pressure rather than intense pain.
2) Shortness of Breath:
- Men: Difficulty breathing or breathlessness.
- Women: May experience more pronounced shortness of breath compared to men.
Unique Symptoms in Women:
1) Pain in the Jaw, Neck, or Back:
- Women: Discomfort in these areas may be a significant indicator.
- Men: While men can experience this, it’s reported more frequently in women.
2) Extreme Fatigue:
- Women: Profound tiredness even with minimal activity.
- Men: Fatigue may be present but is often less extreme.
3) Nausea or Vomiting:
- Women: Gastrointestinal symptoms like nausea and vomiting may occur.
- Men: These symptoms can occur but are reported more commonly in women.
4) Lightheadedness:
- Women: Feeling dizzy or lightheaded may be more prominent.
- Men: While present in both, women may experience it more intensely.
Signs More Common in Men:
1) Radiating Arm Pain:
- Men: Pain or discomfort radiating down the left arm.
- Women: This symptom can occur in women but is more frequently reported in men.
2) Chest Pain Intensity:
- Men: May experience more intense chest pain.
- Women: Chest discomfort in women is often described as pressure rather than severe pain.
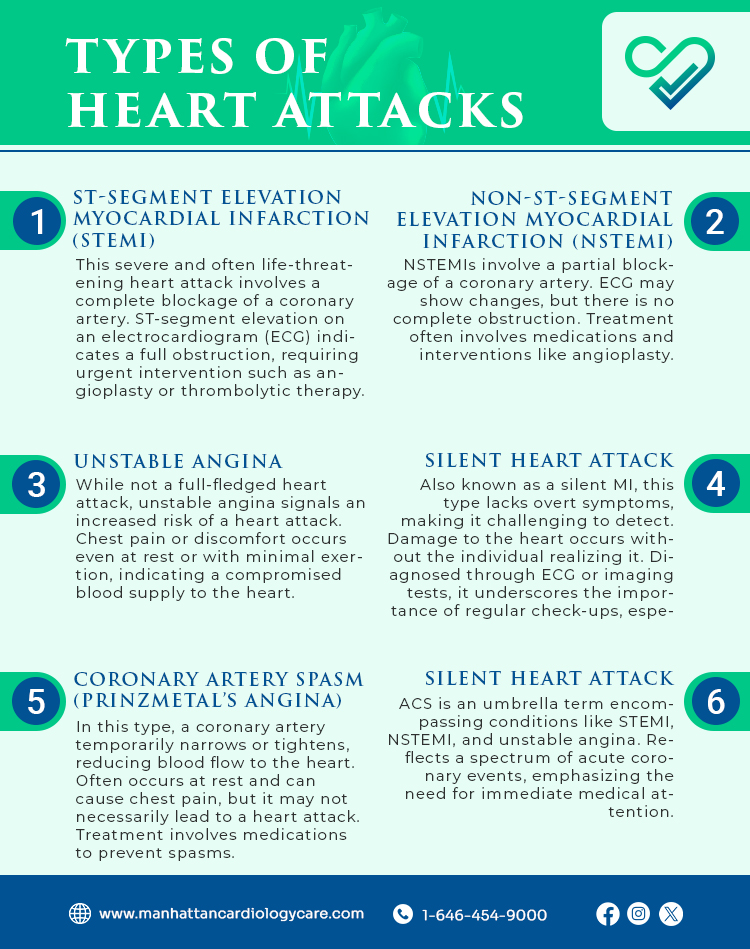
Types of Heart Attacks
Heart attacks, or myocardial infarctions, can manifest in different forms, each with its unique characteristics. Understanding these types is vital for medical intervention.
Here are the main classifications:
-
ST-Segment Elevation Myocardial Infarction (STEMI):
This severe and often life-threatening heart attack involves a complete blockage of a coronary artery. ST-segment elevation on an electrocardiogram (ECG) indicates a full obstruction, requiring urgent intervention such as angioplasty or thrombolytic therapy.
-
Non-ST-Segment Elevation Myocardial Infarction (NSTEMI):
NSTEMIs involve a partial blockage of a coronary artery. ECG may show changes, but there is no complete obstruction. Treatment often involves medications and interventions like angioplasty.
-
Unstable Angina:
While not a full-fledged heart attack, unstable angina signals an increased risk of a heart attack. Chest pain or discomfort occurs even at rest or with minimal exertion, indicating a compromised blood supply to the heart.
-
Silent Heart Attack:
Also known as a silent MI, this type lacks overt symptoms, making it challenging to detect. Damage to the heart occurs without the individual realizing it. Diagnosed through ECG or imaging tests, it underscores the importance of regular check-ups, especially for those at risk.
-
Coronary Artery Spasm (Prinzmetal’s Angina):
In this type, a coronary artery temporarily narrows or tightens, reducing blood flow to the heart. Often occurs at rest and can cause chest pain, but it may not necessarily lead to a heart attack. Treatment involves medications to prevent spasms.
-
Acute Coronary Syndrome (ACS):
ACS is an umbrella term encompassing conditions like STEMI, NSTEMI, and unstable angina. Reflects a spectrum of acute coronary events, emphasizing the need for immediate medical attention.
Causes of Heart Attack
A heart attack is often the result of a combination of factors contributing to the blockage of blood flow to the heart muscle. Understanding these causes is essential for preventive measures. Diet After Heart Attack The risk factors for heart attacks include high blood pressure, high cholesterol, diabetes, smoking, obesity, and a sedentary lifestyle. Addressing these risk factors through lifestyle changes and medical treatment can significantly reduce the chances of experiencing a heart attack
Here are the primary contributors:
The most common cause of heart attacks, CAD involves the accumulation of fatty deposits (atherosclerosis) in the coronary arteries.
-
Plaque Rupture:
Rupture or erosion of a plaque within a coronary artery can trigger the formation of blood clots. Clots can block blood flow, leading to a heart attack.
-
Blood Clot Formation:
Formation of a blood clot within a coronary artery obstructs blood flow.
-
Coronary Artery Spasm:
Sudden, temporary narrowing of a coronary artery, reducing blood supply to the heart. Emotional stress, drug use, or exposure to cold can induce spasms, potentially leading to a heart attack.
-
Atherosclerosis:
Progressive buildup of fatty deposits, cholesterol, and other substances in the arterial walls. Constricts arteries, limiting blood flow and increasing the risk of heart attack.
-
Diabetes:
Chronic high blood sugar levels associated with diabetes contribute to blood vessel damage. Accelerates atherosclerosis and raises the risk of heart attack.
-
High Blood Pressure (Hypertension):
Elevated blood pressure strains the heart and damages arteries over time. Weakens blood vessel walls, promoting plaque buildup and increasing the risk of a heart attack.
-
Smoking:
Tobacco smoke contains chemicals that damage blood vessels and promote atherosclerosis.
How is a Heart Attack Diagnosed?
Accurate and prompt diagnosis of a heart attack is critical for effective treatment and improved outcomes. Various diagnostic methods help healthcare professionals determine the presence and severity of a heart attack.
- Electrocardiogram (ECG or EKG): Non-invasive test recording heart’s electrical activity, detecting rhythm abnormalities, identifying heart attack patterns like ST-segment elevation (STEMI) or other changes (NSTEMI).
- Blood Tests: Measures cardiac biomarkers released during a heart attack, with elevated troponin, CK, and myoglobin levels confirming myocardial damage.
- Coronary Angiography: Involves catheter injecting contrast dye into coronary arteries, revealing blockages and guiding treatment decisions.
- Echocardiogram: Ultrasound creating detailed heart images, assessing damage, evaluating ejection fraction, and identifying abnormalities.
- Cardiac MRI (Magnetic Resonance Imaging): Specialized imaging for detailed heart pictures, assessing function, identifying damage, and guiding treatment.
- CT Angiography: Produces cross-sectional heart and vessel images, visualizing arteries, detecting blockages, and assessing cardiac anatomy.
- Exercise Stress Test: Measures heart response to physical exertion, evaluating function, identifying abnormalities, and revealing reduced blood flow.
- Nuclear Stress Test: Involves injecting radioactive material for stress imaging, highlighting reduced blood flow areas and aiding coronary artery disease assessment.
- Chest X-ray: X-rays capturing heart and lung images, identifying abnormalities like an enlarged heart or lung fluid associated with a heart attack.
- Ambulatory ECG Monitoring (Holter Monitoring): Portable devices recording heart activity, capturing intermittent abnormalities not detected in a standard ECG.
Treatment Options for Heart Attack
Swift and effective treatment is important when it comes to managing a heart attack.
Here are the key treatment options:
- Medications: Various medications address different aspects of a heart attack, including antiplatelet drugs, anticoagulants, beta-blockers, and ACE inhibitors, to reduce blood clotting, lower blood pressure, and improve heart function.
- Percutaneous Coronary Intervention (PCI) or Angioplasty: A catheter with a balloon opens a blocked artery, often with a stent, rapidly restoring blood flow to the heart muscle, reducing damage, and improving outcomes.
- Thrombolytic Therapy: Intravenous drugs (thrombolytics) dissolve blood clots, effectively restoring blood flow when PCI is not immediately available, particularly in remote or rural settings.
- Coronary Artery Bypass Grafting (CABG): A surgical procedure involving grafting blood vessels to bypass blocked coronary arteries, reserved for complex cases or when multiple arteries are affected, providing a long-term solution to restore blood flow.
- Oxygen Therapy: Supplemental oxygen increases oxygen levels in the blood, helping relieve strain on the heart and improving oxygen supply to damaged tissues.
- Antiplatelet Therapy: Medications like aspirin or clopidogrel inhibit platelet aggregation, reducing the risk of further clot formation, essential for preventing recurrent cardiovascular events.
- Statins: Cholesterol-lowering medications reduce the risk of further plaque formation and stabilize existing plaques.
- Beta-Blockers: Medications that block the effects of adrenaline on the heart, helping lower blood pressure, heart rate, and workload on the heart.
- Angiotensin-Converting Enzyme (ACE) Inhibitors: Medications that relax blood vessels and lower blood pressure, particularly beneficial in preventing further damage to the heart muscle.
- Cardiac Rehabilitation: A structured program involving exercise, education, and counseling aids recovery, improves heart health, and reduces the risk of future cardiac events.
– Disclaimer –
This blog is for informational & educational purposes only, and does not intend to substitute any professional medical advice or consultation. For any health related concerns, please consult with your physician, or call 911.