Have you ever experienced or seen what it’s like to care for someone who is experiencing a heart failure?
Going through a heart failure and the consequent heart failure treatments is challenging for both patient and the caregiver. And in order for the caregiver to provide sufficient support, it requires them to have in-depth understanding of the condition.
Today’s blog is a guide for caregivers, where we’ll explore what is heart failure, by navigating its types, signs of heart failure, its symptoms, stages, and risk factors, along with heart failure treatments.
Table of contents
What is Heart Failure?
Heart failure is a complex and often misunderstood condition where the heart is unable to pump blood effectively, compromising the body’s vital functions. Contrary to its name, heart failure doesn’t mean the heart has stopped working – it just struggles to meet the body’s demands for oxygen and nutrients. Here is the common Types of Heart Failure:
Types of Heart Failure
Systolic vs Diastolic Heart Failure
- Systolic Heart Failure:
Systolic heart failure occurs when the heart’s pumping ability weakens, leading to reduced blood ejection from the left ventricle. This results in insufficient oxygen supply to the body’s tissues. - Diastolic Heart Failure:
Diastolic heart failure is characterized by the heart’s inability to relax and fill with blood during the resting phase, impacting its ability to pump effectively. Both types present unique challenges and require tailored approaches to management.
What Causes Heart Failure?
Here are the main factors that can lead to heart failure:
- Coronary Artery Disease (CAD): CAD occurs when the blood vessels supplying the heart muscle become narrowed or blocked. This restricts blood flow and can result in damaged heart muscle.
- Hypertension (High Blood Pressure): Prolonged high blood pressure puts strain on the heart, gradually weakening its muscle and diminishing its pumping efficiency.
- Diabetes Mellitus: Diabetes can lead to damage of the blood vessels and nerves, affecting the heart’s blood supply and overall function.
- Valvular Heart Diseases: Malfunctioning heart valves can impede the smooth flow of blood through the heart, forcing it to work harder, which weakens the heart.
- Cardiomyopathy: Conditions that directly affect the heart muscle, such as cardiomyopathy, can weaken the heart’s pumping ability.
- Myocardial Infarction (Heart Attack): Experiencing and surviving a heart attack increases the risk of subsequent heart failure.
- Genetic Factors: Family history plays a role in heart health. If close relatives have a history of heart failure or cardiovascular diseases, an individual’s risk may be elevated.
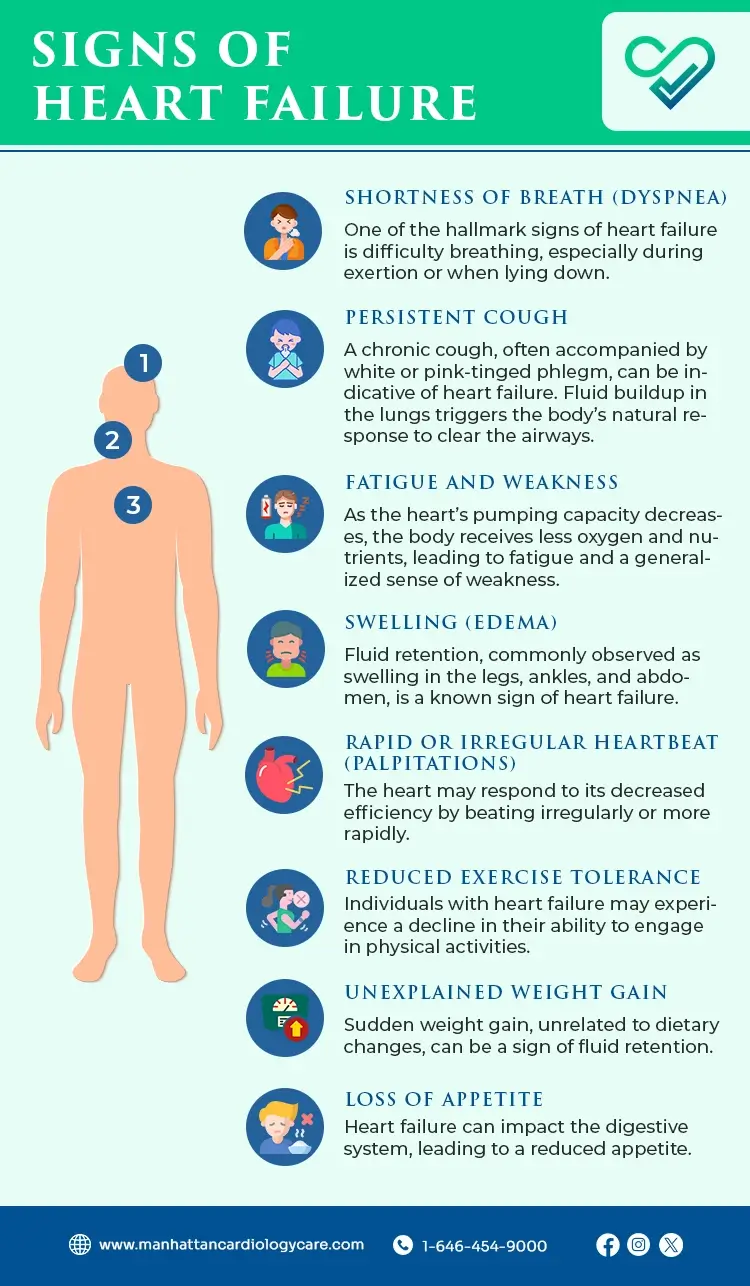
Signs of Heart Failure
Recognizing the signs of heart failure is important for timely intervention and effective management.
- Shortness of Breath (Dyspnea): One of the hallmark signs of heart failure is difficulty breathing, especially during exertion or when lying down.
- Persistent Cough: A chronic cough, often accompanied by white or pink-tinged phlegm, can be indicative of heart failure. Fluid buildup in the lungs triggers the body’s natural response to clear the airways.
- Fatigue and Weakness: As the heart’s pumping capacity decreases, the body receives less oxygen and nutrients, leading to fatigue and a generalized sense of weakness.
- Swelling (Edema): Fluid retention, commonly observed as swelling in the legs, ankles, and abdomen, is a known sign of heart failure.
- Rapid or Irregular Heartbeat (Palpitations): The heart may respond to its decreased efficiency by beating irregularly or more rapidly.
- Reduced Exercise Tolerance: Individuals with heart failure may experience a decline in their ability to engage in physical activities.
- Unexplained Weight Gain: Sudden weight gain, unrelated to dietary changes, can be a sign of fluid retention.
- Loss of Appetite: Heart failure can impact the digestive system, leading to a reduced appetite.
Heart Failure vs Congestive Heart Failure
Heart failure and congestive heart failure are terms often used interchangeably, but here’s how they’re different:
- Heart Failure:
Heart failure is a broad term encompassing the heart’s inability to pump blood effectively, leading to insufficient oxygen delivery to the body’s tissues. It doesn’t necessarily imply the heart has stopped working, it just struggles to meet the body’s demands. - Congestive Heart Failure (CHF):
Congestive heart failure is a specific type of heart failure where fluid builds up around the heart and other organs, causing congestion. This fluid retention can lead to symptoms such as swelling (edema) in the extremities and lungs, resulting in difficulty breathing.
Risk Factors of Heart Failure
The risk factors for heart failure include:
- Hypertension (High Blood Pressure)
- High Cholesterol
- Diabetes Mellitus
- Smoking
- Obesity and Overweight
- Physical Inactivity
- Family History of Heart Disease
- Excessive Alcohol Consumption
- Stress
Stages of Heart Failure
Heart failure is a progressive condition that evolves through stages, each signifying a different level of severity.
Stage I: Mild Heart Failure (Class I)
In this initial stage, individuals may not experience noticeable signs of heart failure during regular physical activity. Heart function remains relatively normal, and the individual can carry out daily tasks without significant limitations.
Stage II: Moderate Heart Failure (Class II)
At this stage, early signs of heart failure become more apparent during exertion. While individuals can manage routine activities, increased physical effort may lead to fatigue, shortness of breath, or palpitations.
Stage III: Severe Heart Failure (Class III)
As it progresses to severe heart failure, symptoms intensify, even with minimal physical activity. Individuals may experience discomfort and limitations in their daily lives. Shortness of breath, fatigue, and reduced exercise tolerance become more pronounced.
Stage IV: End-Stage Heart Failure (Class IV)
In this end stage heart failure, symptoms are persistent and severe, even at rest. Quality of life is significantly compromised, and individuals may require advanced medical interventions, such as heart transplantation or mechanical circulatory support.
Heart Failure Diagnosis
Here’s an overview of the various methods used for heart failure diagnosis:
- Medical History and Physical Examination: The diagnostic process begins with a thorough review of medical history and a detailed physical examination. Healthcare providers assess symptoms, lifestyle factors, family history, and vital signs, checking for signs of fluid retention.
- Blood Tests: Blood tests provide crucial information about heart health. Measurement of B-type natriuretic peptide (BNP) levels gauges the severity of heart failure. Additional tests, including electrolyte levels and kidney function, offer insights into potential contributing factors.
- Chest X-ray: A chest X-ray visualizes the heart and lungs, identifying signs of heart enlargement, fluid buildup in the lungs, or other structural abnormalities indicative of heart failure.
- Electrocardiogram (ECG or EKG): An ECG records the heart’s electrical activity, detecting irregularities in rhythm and signs of damage. Abnormal patterns may suggest conditions contributing to heart failure, such as coronary artery disease or prior heart attacks.
- Echocardiogram: Echocardiography, using sound waves, creates a detailed image of the heart’s structure and function. It provides information on pumping capacity, valve function, and structural abnormalities.
- Stress Test: Stress tests monitor the heart’s response to increased physical activity, uncovering abnormalities that may not be apparent at rest. This can be induced through exercise or medication.
- Cardiac Catheterization: Invasive procedures like cardiac catheterization involve threading a catheter through blood vessels to directly measure blood pressure, assess coronary arteries, and inject contrast dye for detailed imaging.
- MRI or CT Scans: Advanced imaging techniques, such as MRI or CT scans, offer detailed images of the heart and surrounding structures, providing valuable information for a comprehensive heart failure diagnosis.
- Holter Monitor or Event Recorder: Ambulatory monitoring devices like Holter monitors or event recorders assess heart rhythm irregularities by continuously recording heart activity over an extended period, capturing sporadic abnormalities.
Heart Failure Treatments
The various options for heart failure treatments include:
-
Medications:
- Angiotensin-Converting Enzyme (ACE) Inhibitors: These medications help relax blood vessels, reducing strain on the heart and improving blood flow.
- Beta-Blockers: By slowing the heart rate and reducing blood pressure, beta-blockers lessen the workload on the heart and improve its efficiency.
- Diuretics: Diuretics, or water pills, help eliminate excess fluid from the body, alleviating symptoms such as swelling and shortness of breath.
- Aldosterone Antagonists: These drugs help regulate salt and water balance, reducing stress on the heart.
- Angiotensin II Receptor Blockers (ARBs): Similar to ACE inhibitors, ARBs relax blood vessels, improving blood flow and reducing strain on the heart.
-
Lifestyle Modifications:
- Dietary Changes: A heart-healthy diet low in sodium and saturated fats can help manage heart failure. Monitoring fluid intake is also crucial.
- Regular Exercise: Under the guidance of healthcare professionals, tailored exercise programs can improve heart function and overall well-being.
- Smoking Cessation: Quitting smoking is essential for heart health, as smoking exacerbates heart failure symptoms.
- Weight Management: Maintaining a healthy weight reduces the workload on the heart and contributes to better overall health.
-
Device Therapy:
- Implantable Cardioverter-Defibrillators (ICDs): ICDs monitor heart rhythm and deliver electric shocks if dangerous arrhythmias are detected.
- Cardiac Resynchronization Therapy (CRT): This involves the use of a pacemaker to coordinate the contractions of the heart’s chambers, improving efficiency.
-
Surgical Interventions:
- Coronary Artery Bypass Grafting (CABG): In cases of coronary artery disease, CABG can restore blood flow to the heart muscle.
- Heart Valve Repair or Replacement: Addressing malfunctioning heart valves can improve overall heart function.
- Ventricular Assist Devices (VADs): These mechanical devices can support the heart’s pumping function in advanced heart failure.
- Heart Transplantation: For select individuals with severe heart failure, heart transplantation may be considered.
-
Palliative and Supportive Care:
- Palliative Care: Focuses on relieving symptoms, improving quality of life, and providing emotional support.
- End-of-Life Care Planning: In advanced stages, discussions about end-of-life preferences and care planning become essential for patients and their families.
When to See a Doctor?
Early intervention is key in managing heart failure. Caregivers should be vigilant and seek medical attention if they observe worsening symptoms, sudden weight gain, or increased difficulty in breathing. Regular check-ups and open communication with healthcare professionals contribute to effective disease management.
– Disclaimer –
This blog is for informational & educational purposes only, and does not intend to substitute any professional medical advice or consultation. For any health related concerns, please consult with your physician, or call 911.