Table of contents
What is Constrictive Pericarditis?
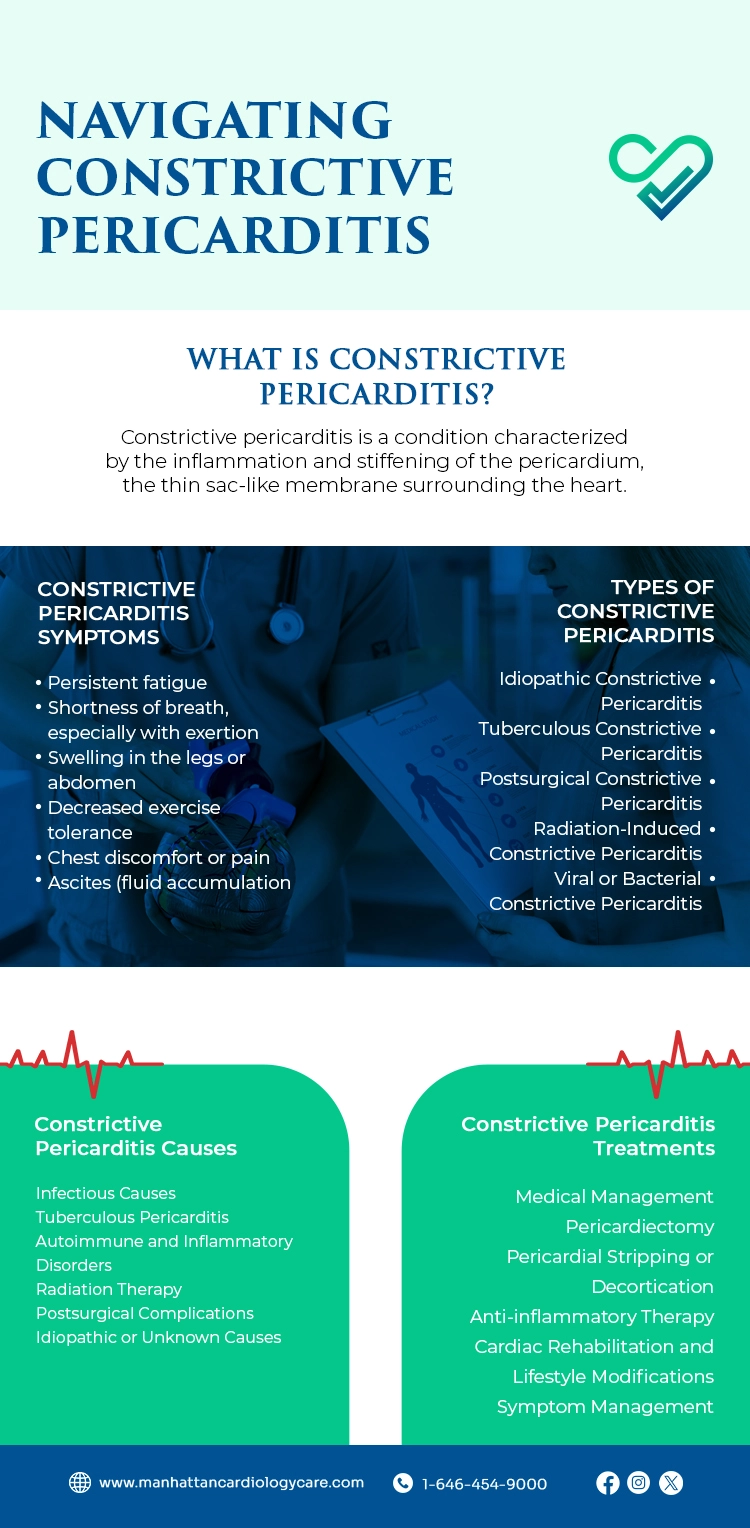
Constrictive pericarditis is a condition characterized by the inflammation and stiffening of the pericardium, the thin sac-like membrane surrounding the heart.
Normally, the pericardium is flexible, allowing the heart to beat and function smoothly. However, when it becomes thickened and rigid due to inflammation, it constricts the heart’s movement, impairing its ability to pump blood efficiently.
Difference Between Restrictive & Constrictive Pericarditis
While both constrictive and restrictive pericarditis involve abnormalities of the pericardium, they have distinct characteristics.
Constrictive pericarditis is marked by the thickening and rigidity of the pericardium, leading to impaired cardiac function. Cardiac test This condition can be challenging to diagnose, as the symptoms may resemble other heart diseases. Diagnostic tests, such as imaging scans and hemodynamic measurements, are crucial in confirming the diagnosis and determining the appropriate treatment approach. Early detection and management of constrictive pericarditis are essential to prevent further complications and improve patient outcomes.
On the other hand, restrictive pericarditis involves the stiffening of the pericardium without significant constriction, resulting in reduced heart filling capacity.
How Common is Constrictive Pericarditis?
Constrictive pericarditis is considered rare compared to other cardiac conditions. However, its incidence may be underestimated due to its often subtle and insidious onset. While it can affect individuals of any age, it is more commonly diagnosed in adults, particularly those with a history of prior pericardial inflammation or surgery.
Constrictive Pericarditis Symptoms
The constrictive pericarditis symptoms can vary widely and may mimic those of other cardiac or respiratory conditions.
Common constrictive pericarditis symptoms include:
- Persistent fatigue
- Shortness of breath, especially with exertion
- Swelling in the legs or abdomen
- Decreased exercise tolerance
- Chest discomfort or pain
- Ascites (fluid accumulation in the abdomen)
Types of Constrictive Pericarditis
Constrictive pericarditis can be classified into various types based on its underlying etiology and clinical presentation. These include:
- Idiopathic Constrictive Pericarditis: Idiopathic constrictive pericarditis refers to cases where the exact cause of pericardial inflammation and constriction is unknown. Management involves symptom relief and supportive care tailored to the patient’s needs.
- Tuberculous Constrictive Pericarditis: Tuberculous constrictive pericarditis occurs as a complication of tuberculosis (TB) infection, leading to chronic inflammation and scarring of the pericardium. Management includes anti-tuberculosis medications and pericardiectomy in severe cases.
- Postsurgical Constrictive Pericarditis: Postsurgical constrictive pericarditis develops after cardiac surgery or pericardial procedures, resulting in inflammation and fibrosis. Treatment options vary based on severity and may include medical therapy, pericardiectomy, or pericardial stripping.
- Radiation-Induced Constrictive Pericarditis: Radiation-induced constrictive pericarditis is a complication of thoracic radiation therapy for malignancies, causing fibrosis and constriction of the heart. Management involves symptomatic relief and close monitoring, with pericardiectomy as a consideration in severe cases.
- Viral or Bacterial Constrictive Pericarditis: Viral or bacterial constrictive pericarditis results from acute infections triggering inflammation and impaired cardiac function. Management focuses on treating the underlying infection with appropriate antimicrobial therapy and supportive care.
Constrictive Pericarditis Causes
The constrictive pericarditis causes are diverse and can include:
- Infectious Causes: Infectious pericarditis stems from various pathogens including viruses (e.g., Coxsackievirus, echovirus), bacteria (e.g., Streptococcus, Staphylococcus), fungi (e.g., Candida), and parasites (e.g., Echinococcus). These infections provoke an inflammatory response, leading to pericardial thickening and fibrosis over time.
- Tuberculous Pericarditis: Tuberculous pericarditis, caused by Mycobacterium tuberculosis, arises as a complication of active pulmonary TB. Chronic inflammation and granuloma formation cause pericardial thickening and calcification, resulting in heart constriction.
- Autoimmune and Inflammatory Disorders: Conditions like rheumatoid arthritis, systemic lupus erythematosus (SLE), and scleroderma may predispose individuals to constrictive pericarditis. The immune system’s attack on the pericardium leads to chronic inflammation, fibrosis, and subsequent constriction, managed with immunosuppressive medications and anti-inflammatory therapy.
- Radiation Therapy: Radiation-induced pericarditis occurs following thoracic radiation therapy for cancers like breast cancer, lung cancer, or lymphoma. Ionizing radiation damages the pericardium, causing fibrosis and constriction. Monitoring for signs of pericardial involvement and symptomatic relief are crucial.
- Postsurgical Complications: Postsurgical constrictive pericarditis can develop after cardiac procedures like pericardiectomy or pericardial biopsy. Surgical manipulation or trauma induces an inflammatory response, leading to pericardial thickening and fibrosis.
- Idiopathic or Unknown Causes: In some cases, the cause of constrictive pericarditis remains unknown despite extensive evaluation. These idiopathic cases may have various underlying mechanisms, including genetic factors or subtle inflammatory processes. Management focuses on constrictive pericarditis symptom relief and personalized supportive care.
Constrictive Pericarditis Treatments
Constrictive pericarditis treatments typically involve a multimodal approach aimed at alleviating symptoms and addressing the underlying cause. The choice of constrictive pericarditis treatment depends on various factors, including the severity of constrictive pericarditis symptoms, underlying etiology, and individual patient characteristics.
Constrictive pericarditis treatment options may include:
- Medical Management: Medical management of constrictive pericarditis focuses on symptom relief and reducing inflammation. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or indomethacin alleviate pericardial inflammation and pain. Diuretics such as furosemide manage fluid retention and peripheral edema associated with impaired cardiac function.
- Pericardiectomy: Pericardiectomy is a surgical procedure aimed at removing part or all of the pericardium to relieve constriction and restore normal cardiac function. It’s the definitive treatment for severe or refractory constrictive pericarditis. Pericardiectomy can be done via conventional open surgery or minimally invasive techniques, depending on the patient’s condition and surgical expertise.
- Pericardial Stripping or Decortication: Pericardial stripping removes the outer layer of the pericardium to alleviate constriction and improve cardiac function. It’s a less invasive option than pericardiectomy and may be considered for cases with extensive pericardial fibrosis but no need for complete removal. Pericardial stripping can be done via thoracotomy or thoracoscopy.
- Anti-inflammatory Therapy: Anti-inflammatory therapy targets pericardial inflammation to alleviate symptoms and slow disease progression. Corticosteroids like prednisone or methylprednisolone may be used to reduce inflammation and fibrosis. Long-term use requires careful monitoring due to potential adverse effects.
- Cardiac Rehabilitation and Lifestyle Modifications: Cardiac rehabilitation programs include exercise training, dietary changes, and lifestyle counseling to manage constrictive pericarditis. Regular physical activity improves cardiovascular fitness and quality of life. Dietary modifications, like sodium restriction, help control fluid retention and optimize cardiac function.
- Symptom Management: Constrictive pericarditis symptom management strategies include pain relief with analgesics, using compression stockings or elevating legs for peripheral edema, and providing supplemental oxygen for hypoxemia. Invasive procedures like paracentesis or thoracentesis may be necessary for symptomatic relief of ascites or pleural effusions due to cardiac dysfunction.
– Disclaimer –
This blog is for informational & educational purposes only, and does not intend to substitute any professional medical advice or consultation. For any health related concerns, please consult with your physician, or call 911.