Do you ever stop to wonder about the constant rhythmic beating that echoes in your chest – the consistant and steady beat that is practically keeping you alive?
Your heart – being the most integral part of any functional body, plays the role of pumping blood around the entire body, to maintain life within you. But what would happen if our heart goes through a challenging condition that obstructs its functioning?
In today’s blog, we are offering detailed information on a common heart condition that affects millions worldwide: Coronary Artery Disease (CAD) – with an objective to equip you all with the knowledge required to effectively and timely manage your health.
Table of contents
What is Coronary Artery Disease?
Coronary Artery Disease is basically a heart condition where the blood vessels that are supplying to the heart muscles become narrow and obstructed. Think of it as traffic jam on the roadways of your cardiovascular system, blocking the smooth flow of the essential nutrients and oxygen that need to reach your heart.
Coronary Artery Disease Types
When it comes to Coronary Artery Disease (CAD), understanding its diverse types is necessary in order to identify and treat it effectively.
Two main types of Coronary Artery Disease are:
1) Stable Ischemic Heart Disease
Key Features:
- Predictable Chest Pain or Discomfort: Those with SIHD often experience chest pain or discomfort, known as angina, typically during physical exertion or times of stress.
- Temporary Relief with Rest or Medication: The discomfort tends to subside with rest or medications, offering a temporary relief. This predictability distinguishes SIHD from its more unpredictable counterpart, Acute Coronary Syndrome.
- Underlying Atherosclerosis: SIHD usually stems from atherosclerosis, a gradual buildup of plaque within the coronary arteries. This buildup narrows the arteries, restricting the flow of oxygen-rich blood to the heart muscle.
2) Acute Coronary Syndrome
Key Features:
- Unpredictable Onset: ACS strikes suddenly and often without warning. The symptoms can be severe and are not necessarily triggered by physical exertion.
- Persistence of Symptoms: Unlike the relief experienced with rest in stable angina, the symptoms of ACS persist and may intensify over time.
- Potential for Heart Damage: ACS can lead to the death of heart muscle cells due to a prolonged lack of blood flow. This can result in irreversible damage if not addressed promptly.
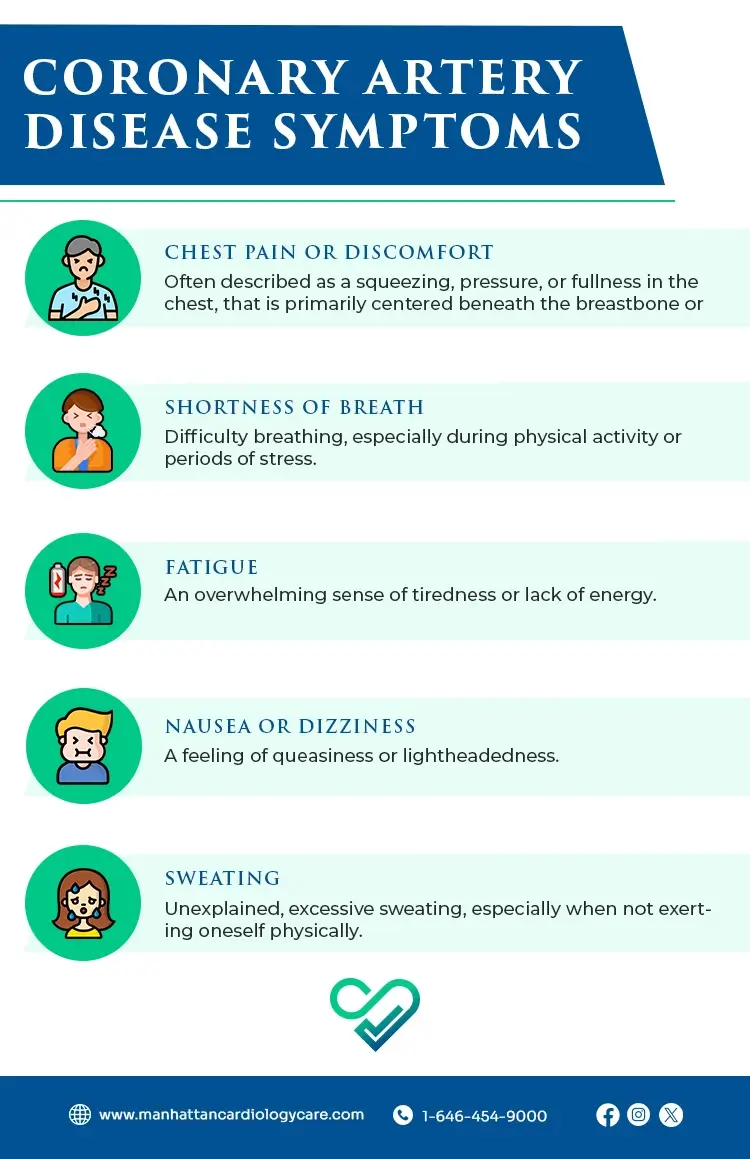
Coronary Artery Disease Symptoms
Being aware of and identifying the Coronary Artery Disease symptoms is essential for timely intervention and effective management of Coronary Artery Disease.
Here are the common Coronary Artery Disease symptoms:
- Chest Pain or Discomfort: Often described as a squeezing, pressure, or fullness in the chest, that is primarily centered beneath the breastbone or slightly to the left.
- Shortness of Breath: Difficulty breathing, especially during physical activity or periods of stress.
- Fatigue: An overwhelming sense of tiredness or lack of energy.
- Nausea or Dizziness: A feeling of queasiness or lightheadedness.
- Sweating: Unexplained, excessive sweating, especially when not exerting oneself physically.
Coronary Artery Disease Causes
Understanding the Coronary Artery Disease causes carries immense importance when it comes to navigating this cardiovascular condition, determining the appropriate Coronary Artery Disease treatment option.
Coronary Artery Disease causes are as follows:
- Atherosclerosis: At the heart of Coronary Artery Disease lies atherosclerosis, a process where the walls of the coronary arteries gradually thicken due to the buildup of cholesterol, fats, and other substances. This arterial narrowing restricts the smooth flow of blood, compromising the vital oxygen supply to the heart muscle.
- High Blood Pressure: Elevated blood pressure places undue stress on the arterial walls, contributing to their gradual hardening and thickening. This constant strain weakens the arteries, setting the stage for atherosclerosis.
- Smoking: Smoking is a major risk factor for this condition. The harmful chemicals in tobacco smoke not only reduce good cholesterol (HDL) but also promote the formation of fatty deposits in the arteries, accelerating the progression of atherosclerosis.
- Diabetes: Individuals with diabetes face an increased risk of Coronary Artery Disease. The elevated blood sugar levels associated with diabetes can damage the arteries, fostering atherosclerosis and increasing the chances of heart complications.
- High Cholesterol: Elevated levels of low-density lipoprotein (LDL) cholesterol, often referred to as “bad cholesterol,” contribute to the buildup of plaque in the arteries.
- Obesity: Carrying excess weight strains the heart and exacerbates other risk factors for CAD, such as high blood pressure, diabetes, and high cholesterol.
Risk Factors for Coronary Artery Disease
Knowing the risk factors for Coronary Artery Disease can massively help with the prevention efforts. These include:
- Age
- Family history
- Smoking
- Poor diet
- Physical inactivity
How is Coronary Artery Disease Diagnosed?
Early and accurate diagnosis is the base for successful Coronary Artery Disease treatment.
– Diagnostic Tests for Coronary Artery Disease
- Electrocardiogram (ECG or EKG): An Electrocardiogram is a foundational test that records the electrical activity of the heart. Electrodes placed on the skin create a visual representation of the heart’s rhythms, helping healthcare professionals identify irregularities and potential signs of Coronary Artery Disease.
- Stress Testing: Stress testing evaluates the heart’s performance during physical exertion. Whether through treadmill exercises or medication-induced stress, this test helps detect abnormalities in blood flow that may not be apparent at rest, helping in the diagnosis of Coronary Artery Disease.
- Echocardiogram: Using sound waves, an echocardiogram produces a detailed image of the heart’s structure and function. This non-invasive test helps identify areas of the heart that may not be receiving adequate blood supply, offering valuable insights into the presence of Coronary Artery Disease.
- Coronary Angiography: Coronary angiography involves injecting a contrast dye into the coronary arteries and capturing X-ray images. This test provides a precise visual map of blood flow, revealing blockages, narrowings, or other abnormalities that may indicate towards Coronary Artery Disease.
Coronary Artery Disease Treatments
From lifestyle modifications to medical interventions, understanding the various Coronary Artery Disease treatments available is important for your journey to wellness.
Listed below are the Coronary Artery Disease treatment options:
-
Lifestyle Modifications
- Heart-Healthy Diet: Adopting a diet rich in fruits, vegetables, whole grains, and lean proteins – along with limiting saturated and trans fats, cholesterol, and sodium.
- Regular Exercise: Physical activity not only helps manage weight but also strengthens the heart. Engaging in moderate aerobic exercises, such as brisk walking or swimming, for at least 150 minutes per week promotes cardiovascular fitness.
- Smoking Cessation: Quitting smoking is a pivotal step in CAD management. The harmful substances in tobacco smoke contribute to the progression of atherosclerosis, and quitting significantly improves heart health.
-
Medications
- Aspirin: Aspirin helps prevent blood clot formation, reducing the risk of heart attacks in individuals with Coronary Artery Disease – However, its use should be under medical supervision due to potential side effects.
- Statins: Statins lowers cholesterol levels, mitigating the buildup of plaque in the arteries.
- Beta-Blockers: Beta-blockers reduce the heart’s workload by slowing the heart rate and lowering blood pressure.
- Nitroglycerin: Nitroglycerin helps relax and widen blood vessels, easing chest pain (angina) in individuals with stable ischemic heart disease.
-
Medical Procedures
- Angioplasty and Stent Placement: In angioplasty, a catheter is used to widen narrowed arteries, often accompanied by the placement of a stent—a small mesh tube—to maintain blood flow.
- Coronary Artery Bypass Grafting (CABG): CABG involves using a healthy blood vessel, typically from the leg or chest, to bypass blocked arteries, restoring proper blood flow to the heart.
Can Coronary Artery Disease be Prevented?
Yes! Fortunately, preventing Coronary Artery Disease is possible through adopting some heart-healthy habits, such as:
- Maintain a balanced diet
- Stay physically active
- Manage stress
- Control blood pressure and cholesterol
When Should I Go to the Doctor
Seeking medical attention for Coronary Artery Disease becomes necessary if you experience:
- Chest pain or discomfort
- Shortness of breath
- Unexplained fatigue
Conclusion
Knowledge regarding the occurring condition is the first line of defense of us all. The more we know about the condition that’s effecting us, the easier t becomes for us to deal with it, along with increasing the chances of taking the right decisions.
At Manhattan Cardiology Care Clinic, we are dedicated to providing personalized care for your heart health. Schedule a consultation today and let’s ensure your heart continues to beat strong.
– Disclaimer –
This blog is for informational & educational purposes only, and does not intend to substitute any professional medical advice or consultation. For any health related concerns, please consult with your physician, or call 911.